Increasing Healthcare Provider Referrals for Diabetes Prevention
Submission Date: September 2014
Entry Type: Case Study
State/Territory Submitted on the Behalf of: Minnesota
States/Territories Involved: Minnesota
Funding Source: NACDD
Other Funding:NACDD funding
Domain Addressed:Community-Clinical Linkages, Health Systems Strategies
Public Health Issue:86 million (more than 1 out of 3) American adults have prediabetes, and 9 out of 10 people with prediabetes do not know they have it. Without lifestyle changes to improve their health, 15 – 30% of people with prediabetes will develop type 2 diabetes within five years.
The Diabetes Prevention Program research study showed that making modest behavior changes helped participants lose 5 – 7% of their body weight and reduced the risk of developing type 2 diabetes by 58% in people with prediabetes.
Many healthcare providers are not currently referring to the National Diabetes Prevention Program’s (National DPP) evidence-based lifestyle change program. One strategy to promote referrals to the lifestyle change program is to work with healthcare providers and practices to help providers easily refer their patients to the program.
Project Objectives:Increase the number of providers trained to refer patients to the We Can Prevent Diabetes project from 7 to 114 and increase the number of adult patients referred to the evidence-based lifestyle change program in WCPD from 0 to 710 by December 31, 2013.
Program Action:The Minnesota Department of Health (MDH) worked with healthcare providers and staff at 24 clinics involved in the We Can Prevent Diabetes (WCPD) Minnesota research study. This CMS-funded study uses the YMCA Diabetes Prevention Program (Y-DPP) as its evidence-based lifestyle change program and tests the effects of incentives on attendance and weight loss among Medicaid enrollees in the Y-DPP. Through existing partnerships, the MDH worked synergistically with WCPD clinics to increase provider awareness and incorporate community feedback to support enrollment in the Y-DPP. The MDH used CMS funds to provide clinic trainings as part of the WCPD study. The State Diabetes Prevention Project funds were used to support healthcare provider discussions about identification of patients with prediabetes, referral to the Y-DPP, and how to tailor recruitment strategies for diverse communities.
State Health Department Roles
- Formed strategic partnerships with and provided guidance to WCPD healthcare organizations and their clinics to increase referrals to the evidence-based lifestyle change program
- Contracted with an experienced consultant to facilitate healthcare provider discussions at WCPD clinics
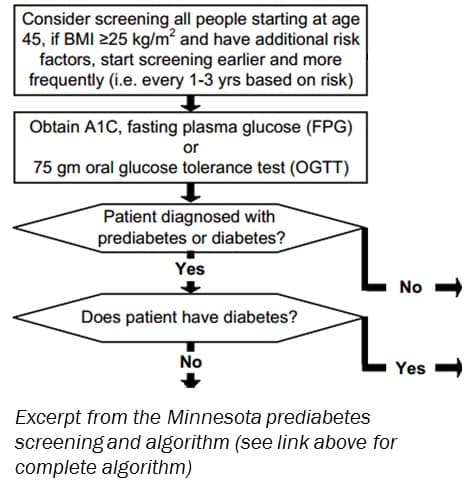
- Provided current information to the WCPD clinics, including an updated prediabetes treatment and referral algorithm, provider referral card, and a list of evidence-based lifestyle change program providers
- Invited WCPD clinics to attend community conversations with African American, American Indian, Latino, Asian/Hmong, and Somali groups
- Worked with WCPD clinics to plan and conduct community health and resource fairs aimed at increasing referrals to the evidence-based lifestyle change program
Partners
- We Can Prevent Diabetes/Medicaid Incentives for Prevention of Chronic Disease study clinics and clinic coordinators
- Contract consultant
To generate healthcare provider referrals at WCPD clinics, the MDH held provider discussions facilitated by a contract consultant who is a well-known Certified Diabetes Educator. Slides used during discussions were adapted from a healthcare provider webinar, which highlighted a healthcare provider toolkit and a recently updated prediabetes screening and treatment algorithm (http://icanpreventdiabetes.org/health-provider-toolkit/). The discussions provided a forum to explore barriers as well as policy or practice changes for referring patients to the evidence-based lifestyle change program. Policy or system changes varied and included use of:
- Electronic medical records to flag patients at risk for prediabetes based on an algorithm
- Standing orders for labs so that patients at risk for prediabetes could be screened immediately
- Risk assessment screening tools
- Clinic flow sheets outlining steps from identification to enrollment in the lifestyle change program
- WCPD clinic coordinators to explain the program to patients at risk for prediabetes
- Positive language to describe the program
Several tools were developed as a result of the discussions, including a 3 x 5 inch provider pocket card, patient handouts translated into three languages, and risk assessment pads. In addition, new insights obtained from conversations with five ethnic communities were shared during provider discussions. With respect for providers’ knowledge of their patient populations, these insights were used to strategize ways to recruit patients from diverse communities. The MDH also invited WCPD clinics to attend community conversations to learn about culturally acceptable recruitment, enrollment, and implementation of evidence-based lifestyle change programs. Clinics added value to the discussion by sharing their perspectives about the patient populations they serve. Furthermore, the WCPD clinic coordinators formed a partnership to increase referrals within and across each of their clinics. The MDH hosted partnership meetings, which was helpful for scheduling provider discussions and moving forward with policy and practice changes.
“Each participating clinic receives funds for a staff position responsible for recruitment and enrollment in the WCPD study. This person works with providers and other clinic staff to develop policies and systems for referral to the Y-DPP. This position is important for success.” Gretchen Taylor, MDH
Impact/Accomplishments:- 13 Healthcare system partners
- 24 Healthcare delivery sites
- 114 Primary care health providers
- 48,679 Adult patients served by these providers
- 560 Adult patients referred to evidence-based lifestyle change program
- 7 Provider discussions
- 88 Healthcare providers attended discussions
Factors Supporting Success
- Dedicated Funding: $42,656
- Centers for Medicare & Medicaid Services grant funding for the WCPD study
- Connections to healthcare systems and clinics participating in the WCPD study
- Experience with the evidence-based lifestyle change program
- Awareness of cultural commonalities and differences
- Facilitated learning opportunities between WCPD clinics, providers, and coordinators across systems and sites
- MDH WCPD Project Coordinator established and strengthened relationships with WCPD clinics
- Accessed WCPD clinic coordinator partnership to schedule provider discussions and strengthen referral processes
- WCPD clinic coordinators passionately promoted the evidence-based lifestyle change program and diabetes prevention
- Utilized insight from community conversations to strategize for program recruitment and implementation
Challenges and Solutions
- Challenge: Not all WCPD clinics had a robust referral system
- Solution: As a result of the provider discussions, six clinics developed and implemented prediabetes identification and referral processes that included referral to the evidence-based lifestyle change program.
- Challenge: WCPD clinics working to promote and refer patients to the evidence-based lifestyle change program reported challenges engaging patients in a year-long program
- Solution: WCPD Project Coordinator coached individual clinic staff responsible for recruiting about how to reframe the program as “a year of support”
- Solution: Role playing and a brief tutorial on motivational interviewing were used to teach clinic staff how to highlight the positive aspects of the program
- Challenge: WCPD clinic coordinators expressed difficulty generating referrals among certain communities due to a lack of diverse coaches, cultural beliefs, and timing of religious practices
- Solution: MDH used feedback from community conversations to tailor their approach to recruitment; examples include: seeking out representatives from communities to be trained as coaches, scheduling classes around holidays, and focusing on provider referral to increase enrollment
https://www.chronicdisease.org/?ndpp
Diabetes
State Contact Information:
MN
Gretchen Taylor
Minnesota Department of Health
651-201-5390
gretchen.taylor@state.mn.us
