Development of a Diabetes Prevention Referral System
Submission Date: September 2014
Entry Type: Case Study
State/Territory Submitted on the Behalf of: West Virginia
States/Territories Involved: West Virginia
Domain Addressed:Community-Clinical Linkages, Health Systems Strategies
Public Health Issue:In WV, the diabetes prevalence is 13% and the prediabetes prevalence is 8.6%. Without lifestyle changes to improve their health, 15 – 30% of people with prediabetes will develop type 2 diabetes within five years.
The Diabetes Prevention Program research study showed that making modest behavior changes helped participants lose 5 – 7% of their body weight and reduced the risk of developing type 2 diabetes by 58% in people with prediabetes.
Statewide, regional, or system-wide referral systems can connect people with prediabetes to the National Diabetes Prevention Program’s (National DPP) evidence-based lifestyle change program. Developing and implementing systems for referral of people at risk to sites offering the lifestyle change program is a sustainable strategy to increase use of this program.
Project Objectives:To develop and implement a referral system for people with or at risk for prediabetes in a minimum of 4 evidence-based lifestyle change program providers and a minimum of 4 primary care centers.
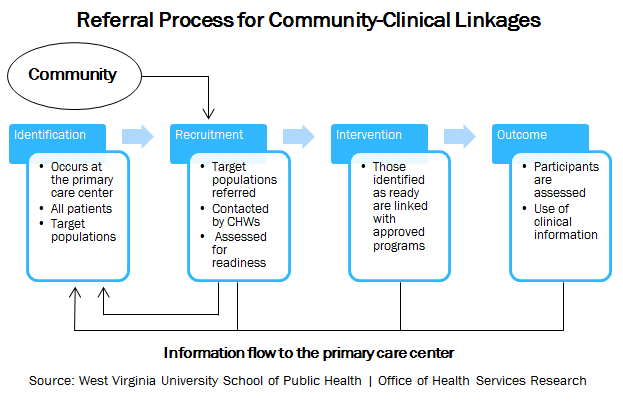
Program Action:An effective diabetes prevention referral system helps ensure optimal care for individuals at risk by connecting them to an evidence-based lifestyle change program provider. The West Virginia Diabetes Prevention and Control Program (DPCP) partnered with West Virginia University Office of Health Services Research (WVU OHSR) to develop a referral system and algorithm for use in health centers. The system they developed included an algorithm for identification of patients at risk for diabetes and intervention through the evidence-based lifestyle change program.
The referral system worked as follows: 1) at-risk patients identified through electronic health record (EHR) data or individual screening, 2) patients informed of their risk and the evidence-based lifestyle change program by the health center or lifestyle change program provider, 3) referral forms returned to lifestyle change program providers and patients provided a copy of the referral, and 4) patients enrolled in program. The DPCP expected these elements to remain relatively uniform across health centers, with slight differences in process and methods of communication used. The algorithm listed procedures for identification of patients at risk for diabetes and referral to the evidence-based lifestyle change program. The algorithm also provided two sets of instructions for follow-up with referred patients who either: a) participated in the program, or b) did not participate or were “no shows.” These follow-up instructions were aimed at both healthcare and lifestyle change program providers (i.e. community health workers) to ensure a closed loop referral and/or intervention. Following development, the referral system and algorithm were pilot tested at three health centers. To ensure there were sufficient lifestyle change program providers for pilot centers to refer patients, the DPCP partnered with WVU Extension and local health departments in Community Transformation Grant (CTG) communities to link health centers to the lifestyle change program providers. Staff from WVU Extension had community-level experience and pre-existing relationships with health centers, which helped connect centers to evidence-based lifestyle change program providers. In addition, a service agreement outlined a partnership between the health center, WVU OHSR, and the evidence-based lifestyle change program provider. The responsibilities of each partner were outlined, with the goal being for at-risk patients to receive the care they need and have that information funnel back to the health center. Forms were created for referral and quarterly review of indicators.
“Helping to identify at-risk patients was only the first step. Helping to build a system whereby those patients could be referred for appropriate care, and that the results and progress of those patients are shared back to the referring physician, was key.”
-Adam Baus, WVU OHSR
State Health Department Roles
- Contracted with WVU OHSR to create a diabetes prevention referral system
- Developed a screening/referral algorithm for prediabetes diagnosis and referral
- Partnered with West Virginia University Extension Service (WVU Extension) and local health departments to connect health centers with evidence-based lifestyle change programs and trained lifestyle change coaches
- Facilitated meetings between health centers and evidence-based lifestyle change program providers in order to establish a formalized referral process
- Drafted a service agreement between health centers and evidence-based lifestyle change program providers
- Linked Federally Qualified Health Centers and evidence-based lifestyle change program providers
- Formed partnerships with WVU Extension Service and local health departments Connected with partners (WVU Extension and CTG local health departments) whose staff had been trained as lifestyle coaches and had pre-existing relationships with their local health centers
- Incorporated referral to the evidence-based lifestyle change program into health centers’ existing delivery systems
Partners
- West Virginia University Office of Health Services Research
- Community Health Centers and Free Clinics
- West Virginia University Extension Service
- Community Transformation Grant Local Health Departments
- 5 Healthcare system partners
- 3,966 Adults with prediabetes living in the area covered by the referral system
- 261 Adults referred to the evidence-based lifestyle change program through the newly created referral system
Factors Supporting Success
- Dedicated Funding: $80,000
- Partnerships with health centers and evidence-based lifestyle change program providers
- 10-year history of quality improvement partnerships with WVU OHSR and health clinics
- Linked Federally Qualified Health Centers and evidence-based lifestyle change program providers
- Formed partnerships with WVU Extension Service and local health departments
- Connected with partners (WVU Extension and CTG local health departments) whose staff had been trained as lifestyle coaches and had pre-existing relationships with their local health centers
- Incorporated referral to the evidence-based lifestyle change program into health centers’ existing delivery systems
Challenges and Solutions
Challenge: Health centers and evidence-based lifestyle change program providers were not always located in the same area
Solution:The DPCP helped link health centers and evidence-based lifestyle change program providers
Challenge: Not all patients referred to the program were previously informed of their prediabetes risk
Solution: Recognized the importance of determining the process for patient contact and education, including the readiness assessment, recruitment, and referral roles
The WV Division of Health Promotion & Chronic Disease will be bringing together diabetes prevention stakeholders to assess progress and determine WV’s next steps.
https://www.chronicdisease.org/?NDPP_WV
Diabetes
State Contact Information:
WV
Jessica Wright and Tony Leach (Tony.M.Leach@wv.gov)
West Virginia Diabetes Prevention and Control Program
304-356-4193
Jessica.G.Wright@wv.gov
