BUILDING HEALTHY MILITARY COMMUNITIES TOOLKIT
A RESOURCE FOR THE DEPARTMENT OF DEFENSE HEALTH PROVIDERS AND COMMUNITIES
Working with Public Health
When addressing the health of the force—especially Service members who do not live on installations—it is beneficial to coordinate and collaborate with state and local public health agencies. Collaboration efforts with them can include both tactical and strategic activities.
- Tactical efforts include programs and services that directly aid Service members and their families. Strategic efforts can include policy changes and are intended to have broader reach and can impact larger numbers of Service members.
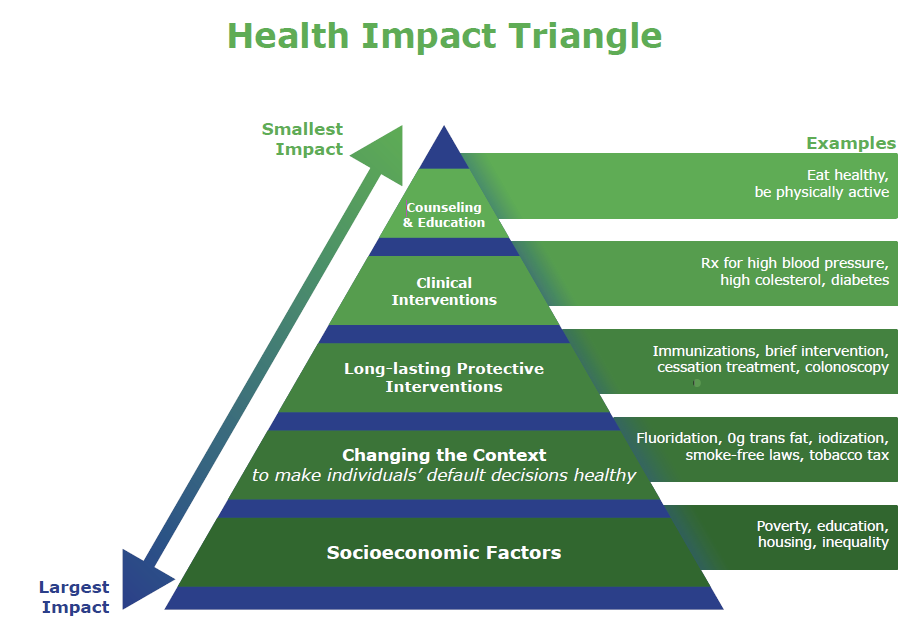
- Strategic efforts can include policy changes and are intended to have broader reach and can impact larger numbers of Service members. Public health professionals call strategies with broader reach the Policy, Systems, and Environmental (PSE) approach. This approach has the potential to make more lasting and significant changes. For example, an installation-wide policy limiting where cigarettes can be smoked will impact many more soldiers than a tobacco cessation aid provided to single Service member.
CDC’s Health Impact Pyramid, shown below, is a five-tier pyramid that describes the impact of different types of public health activities (also called interventions) to improve health. It provides a visualization of how different efforts provide different returns. The interventions listed at the base of the pyramid have the greatest potential impact. These efforts address social and economic factors that influence health. As you move up the pyramid, you find interventions that change the context to make individuals’ default decisions healthy, clinical interventions that require limited contact but provide long-term protection, ongoing direct clinical care, and health education and counseling.¹
The Role of State and Local Health Departments
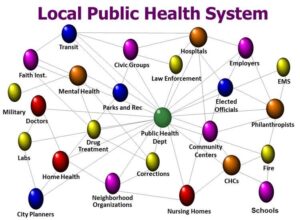
State and local health agencies are ideal first contacts when addressing community health. However, it is important to understand that other entities are critical to collaboration. Together, they comprise a public health system. The public health system is commonly defined as “all public, private, and voluntary entities that contribute to the delivery of essential public health services within a jurisdiction.”1 In addition to health agencies, these groups are also considered as part of the system:
- Healthcare providers
- Public safety agencies
- Human service and charity organizations
- Education and youth development organizations
- Recreation and arts-related organizations
- Economic and philanthropic organizations
- Environmental agencies and organizations
The work of the public health system can be summarized into 10 types of activities or services:
- Monitor health status to identify and solve community health problems
- Diagnose and investigate health problems and health hazards in the community
- Inform, educate, and empower people about health issues
- Mobilize community partnerships and action to identify and solve health problems
- Develop policies and plans that support individual and community health efforts
- Enforce laws and regulations that protect health and ensure safety
- Link people to needed personal health services and assure the provision of health care when otherwise unavailable
- Assure competent public and personal health care workforce
- Evaluate effectiveness, accessibility, and quality of personal and population-based health services
- Research for new insights and innovative solutions to health problems
State Health Improvement Plans
Many state health departments have a state health improvement plan (SHIP). SHIPs are multi-year and identify priorities and strategies for improving health in the state. Most states have a SHIP planning committee that meets to determine progress on the plan and new priorities for the next version of the plan. While most states publish their SHIPs online, some may not. To learn more about a state’s health improvement process and plan, find the state or territory in the Directory of State and Territorial Health Departments and request a copy of the current SHIP. Keep in mind that some states may not have a plan.
SHIPs are data-driven documents and often focus on the Policy, Systems, and Environmental (PSE) work that will have the greatest impact on health. State Health Departments (SHDs) use State Health Assessments (SHA) and other reliable data sources to determine goals and priorities and track progress. As you make the case for prioritizing geographically disbursed Service members in a state’s SHIP, providing data from the Community Readiness Open Data Dashboard (password: mh-dashboard) can help support your case to the planning committee. Contacts for engaging in the SHIP and Community Health Improvement Plans (CHIP) process are discussed below.
Community Health Improvement Plans
Like State Health Improvement Plans, many local jurisdictions publish Community Health Improvement Plans. [Note: Local jurisdictions can be called counties, parishes, or boroughs.] The goals of these plans are made are often based on data from Community or County Health Assessments (CHAs). As with SHIPs, not all local jurisdictions will have a CHIP.
Examples of CHIPs:
How to Connect
- National Association of Chronic Disease Directors
In state health departments, health promotion is typically under the purview of the chronic disease and health promotion bureau. Chronic Disease Directors are ideal as a first connection with your state health department. If you would like a warm introduction to the Chronic Disease Director in a state, The National Association of Chronic Disease Directors can assist. Email info@chronicdisease.org to make your request. - Directory of State and Territorial Health Departments
- Directory of Local Health Offices from the National Association of County and City Health Officials (NACCHO). NACCHO’s improve the health of communities by strengthening and advocating for local health departments.
- In states with centralized or shared governance systems, there is usually an office or division within the state health department that can provide a warm connection to the proper individuals in the local health offices.
- Some states have associations that represent all local health offices in the state. Email contacts and websites for each can be found in NACCHO’s Directory of State Associations of County and City Health Officials.
- The National Indian Health Board represents Tribal governments—both those that operate their own health care delivery systems through contracting and compacting, and those receiving health care directly from the Indian Health Service (IHS).